
Table of Contents
What is Public-Private-Partnership (PPP)?
- A Public-Private Partnership, also called a PPP, P3 or 3P, is an agreement between government agency i.e. local or national government and private sector company.
- Public-Private Partnership refers to the collaboration between government agency and private sector which can be used to finance, build and use projects, usually public projects.
- These partnerships are usually found in transport, municipal and environmental infrastructures and public service accommodation.
Public-Private-Partnership (PPP) in health programs?
- Public-private partnerships in health programs are the encouraging representations for financing successful health care innovations with joint efforts between private and public sectors with a serene concept on partnership structures, common objectives for on-time delivery of the health services.
Importance/Necessity of PPP:
- Timely completion of projects
- Solutions for investing in large projects
- Increased feasibility of the projects/programs
- Enhanced transparency and accountability
- Cost-effectiveness
- Higher productivity and efficiency- by linking payments to performance
- Increased employment opportunities
- Clear customer focus
- Improved customer satisfaction
- Recovery of user charges
- Optimum utilization of resources
- Improvement of quantity and quality of services
- Exchange of expertise among the organizations
Different models of PPP:
Public-Private-Partnership can be of different forms/models. They are:
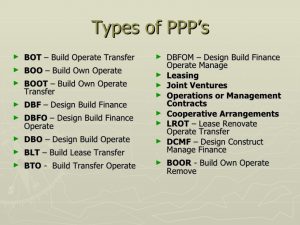
Among these different types/models of PPP, some of them are described as follows:
| Models of PPP | Explanation | Advantages | Limitations |
| Build- Own- Operate- Transfer (BOOT)
|
This model helps to figure out the source of financing, carries out all designs, builds the infrastructure and transfer ownership to the public agency. | · Encourage modernism
· Focus on strengths of PPP · Provide an opportunity to expertise |
· Applicable only for large projects
· High transaction costs · Time-consuming |
| Build- Own- Operate (BOO)
|
In this model, private contractors have control over profits and losses generated by the facility, similar to a privatization process. | · Development of private agency.
· Promotes privatization process |
· Lack of help from public sectors in the financial crisis |
| Build- Operate- Lease- Transfer (BOLT)
|
In this model, the government gives concession to a private entity to build a facility and at the end of the project, transfer of ownership to the government. | · Full authority to government
· Public service delivery in an effective way
|
· Limited motivation for the private sector due to the transfer of ownership |
| Lease -Develop -Operate (LDO)
|
This model involves public owner leasing facility to a private company. The private company responsible for maintenance and operate as per specified. | · Provides a platform for the private sector to perform well. | · No capital mobilized from the private sector |
| Rehabilitate- Operate- Transfer (ROT) | Under this model, the governments and local bodies allow the private agency to rehabilitate facility during concession period and after the period; the project is transferred back to local bodies. | · Provides rehabilitation facility to private promoters. | · Time restriction
|
| Design, Build, Finance and Operate (DBFO)
|
In this model, the private agency undertakes the responsibility for the operation of the project for the period of concession. | · Opens up domestic markets to overseas competition
· Brings new ideas from outside public sector |
· Higher cost of private capital
· Expensive procurement process |
Role of PPP in health programs:
The role of PPP in health programs are:
- Scope of service provider selection through:
- Competitive bidding
- Competitive negotiation
- Risk and revenue sharing
- Market risk arising from insufficient demand
- Implementation risk: delay in project completion, environmental damage
- Finance risk
- Maintenance risk
- Enabling environment
- Leadership from both partners
- Healthy competition to achieve the desired result
- Trust-based contracts
- Achievement of performance indicators
- Periodic review of the progress
- Economic cooperation and integration.
- Cost-effectiveness specially to marginalized people.
- Delivery and management of specified clinical and clinical support services.
- Target achievement with limited investments
- Strong partnership with diverse and dynamic human resource within the team
Limitations of PPP:
- Political and administrative commitment
- Lack of trust on both sides
- Difficultly in administrative and financial management due to differences in policies and working modalities.
- Halfhearted supporters (in some cases)
- Institutional capacity
- Unavailability of appropriate technical and managerial workforce at all levels
- Lack of institutional configurations to manage PPP contracts
- Diversity and complexity of private sector
- Financial barriers leading to payment delays
- Limitation in contract features
- Lack of harmony in supervision and monitoring mechanism
- Need of timely revisions of the contract as per the organizational policy
References and For More Information
https://www.slideshare.net/akhileshbhargava/public-private-partnership-in-health
https://www.slideshare.net/digvijaytrivedi/ppp-in-health
https://marketbusinessnews.com/financial-glossary/public-private-partnership-definition-meaning/
https://www.pwc.com/gx/en/industries/healthcare/publications/trends-for-the-future.html
http://demembranes.com/build-own-operate-boo-build-own-operate-transfer-boot/
https://www.thebalancesmb.com/public-private-partnership-types-845098
McIntosh N, Grabowski A, Jack B, Nkabane-Nkholongo EL, Vian T. A Public-Private Partnership Improves Clinical Performance In A Hospital Network In Lesotho. Health affairs. 2015;34(6):954-62.
Baliga BS, Ravikiran SR, Rao SS, Coutinho A, Jain A. Public-Private Partnership in Health Care: A Comparative Cross-sectional Study of Perceived Quality of Care Among Parents of Children Admitted in Two Government District-hospitals, Southern India. Journal of clinical and diagnostic research : JCDR. 2016;10(2):SC05-9.
